- Home
- Children's education and care
- Manage anaphylaxis risk
Manage anaphylaxis risk
Examples of anaphylaxis risk minimisation strategies for children’s education and care (CEC) services
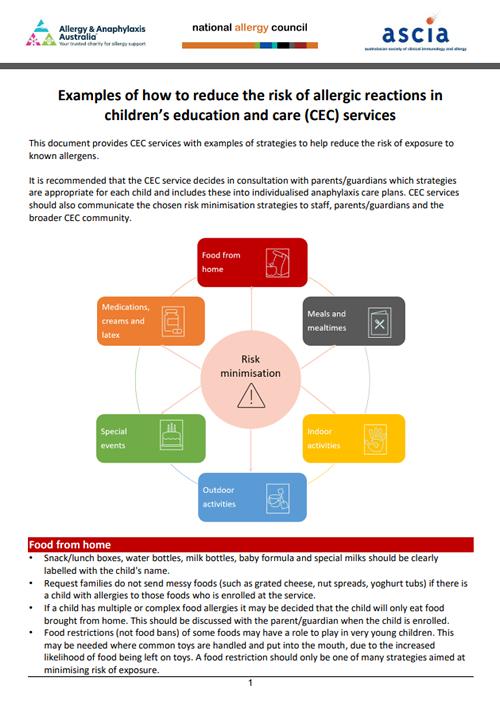
This document provides CEC services with examples of strategies to help reduce the risk of exposure to known allergens.
It is recommended that the CEC service decides in consultation with parents/guardians which strategies are appropriate for each child and includes these into individualised anaphylaxis care plans. CEC services should also communicate the chosen risk minimisation strategies to staff, parents/guardians and the broader CEC community.
Food from home
Snack/lunch boxes, water bottles, milk bottles, baby formula and special milks should be clearly labelled with the child's name.
Request families do not send messy foods (such as grated cheese, nut spreads, yoghurt tubs) if there is a child with allergies to those foods who is enrolled at the service.
If a child has multiple or complex food allergies it may be decided that the child will only eat food brought from home. This should be discussed with the parent/guardian when the child is enrolled.
Food restrictions (not food bans) of some foods may have a role to play in very young children. This may be needed where common toys are handled and put into the mouth, due to the increased likelihood of food being left on toys. A food restriction should only be one of many strategies aimed at minimising risk of exposure.
Meals and mealtime supervision
In cases where children are very young (infants, toddlers) CEC services may choose to have allergen-restricted spaces for children with food allergies to eat, for example, with no egg or cow’s milk (dairy). If this is implemented, children with food allergy should still be able to sit with their peers.
CEC services may choose to exclude foods containing peanuts and tree nuts (such as cashew, hazelnut and almond) in their menu as these are not essential (core) foods and can be eaten at home. Foods which are core foods in the diet such as wheat, cow's milk (dairy) and egg cannot be removed in CEC services.
Discuss menu options and products available with parents/guardians of children with food allergy.
For children with multiple food allergies, it may be necessary to have food and drinks for the child that are checked by parents/guardians. Alternatively, the parents/guardians can provide some or all of the food for their child.
It is suggested that all staff preparing and serving food to children undertake All about Allergens for CEC online training so they understand how to avoid cross contamination during storing, handling, preparing and serving food.
Prepare food for children with food allergy first so their food does not come into contact with other foods being prepared. If the food is to be stored before it is given to the child, it must be clearly labelled with the child’s name and placed in an enclosed container or covered to avoid any contact with other food being stored.
Use easily identified plates, bowls, cups, bottles, cutlery and utensils, using colour and/or a sticker, as well as the child's name. This means staff and children with food allergy can easily identify their food and drink.
Thorough washing of kitchen equipment with hot, soapy water is needed to remove food allergens.
When preparing food, clean/separate utensils should be used.
If shared utensils are used, they should be washed in hot soapy water or the dishwasher to remove traces of potential allergens.
Foods with precautionary allergen labelling statements (such as "may contain traces of…") should not be provided to children allergic to specific foods. They can still be given to other children at the CEC service who do not have those specific food allergies.
Staff supervision is essential at meal and snack times. Where possible, have two staff members check that children with food allergy are given the right food.
If used, have a separate highchair for children with food allergy where possible. This highchair needs to be thoroughly cleaned between children as different children may be allergic to different foods.
Ensure that children do not have access to toys while they are eating.
All children should wash their hands before eating.
Baby wipes can be used to remove allergens from hands (and faces) if running water and soap is not available.
Hand sanitiser should not be used as a substitute to washing hands with soap and water as it does not remove allergens.
Children should always be seated to eat and drink, including babies and toddlers with milk bottles or drinking cups.
Holding babies while they drink their milk can prevent spills.
Using cups with lids will reduce the risk of spills.
Be careful when serving milk (dairy) products that tend to splatter. Foods such as yoghurt tubs and pouches can be avoided to reduce the risk of milk being splattered on surfaces such as tables and chairs.
Children with food allergy should not share, or eat from each other’s plates, bowls, cups, bottles or cutlery.
If using shared platters (such as fruit), give children with food allergy their own separate platter or plate to serve themselves from.
Supervision of children eating is essential, particularly for children with food allergies. However, children who have food allergies should not be isolated from their peers.
Cleaning:
Thoroughly wipe down surfaces of tables, chairs and highchairs, with hot soapy water after meals.
Clean up food and drink spills immediately.
Clean up posits/vomit quickly and thoroughly as they can contain food allergens.
Use disposable paper towels where possible. If cloths are used, machine wash cloths before using again.
Indoor activities
Young children often put their fingers in their mouth, eyes or up their nose, so minimising exposure to food allergens during everyday activities (not just mealtimes) is important.
Games and activities should not involve the use of any foods that children are allergic to.
Cooking activities can present a risk to children with food allergy as common allergens such as milk, egg, wheat are often ingredients.
When cooking or doing activities containing food, talk to parents/guardians well in advance. Where possible known allergens should be substituted with suitable ingredients - parents/guardians of children with food allergy can provide advice.
Wash toys and equipment regularly with hot soapy water. Wind toys and instruments (such as whistles, recorders) are high risk and are best avoided in CEC settings.
Avoid using recycled craft items that could contain food allergens (such as empty plastic milk bottles, egg cartons, cereal boxes, empty peanut and tree nut butter jars, ice cream containers).
Activities such as face painting or mask making (when moulded on the face of the child), should be discussed with parents/guardians prior to the activity, as products used may contain food allergens such as peanut, tree nut, wheat, milk or egg.
Some materials (such as play dough) can contain food allergens.
Discuss options with parents/guardians of children with wheat allergy (such as using wheat-free flour).
Check that nut oils have not been used in the manufacturing process.
If a child with food allergy is unable to use the play dough, provide an alternative material for the child to use and ensure adequate supervision to avoid cross contamination.
Outdoor activities
Insect allergy
Ensure children with insect allergy wear shoes when outside.
Have bee and wasp nests removed by a professional.
Consider poisoning of ant nests if there are children with ant allergy attending (this should only be done when children are not at the centre).
Cover outdoor bins as they attract insects.
Be aware of bees around water and in grassed or garden areas.
Keep lawns and clover mowed.
When purchasing plants, consider those less likely to attract bees and wasps (such as non-flowering plants).
Specify play areas that are lower risk - away from garden beds, flowering plants, water, or garbage storage areas.
Do not have open drink containers outside, particularly those containing sweet drinks, as they may attract stinging insects.
Tick allergy
To reduce the risk of tick bites in tick prone regions, children should wear a hat and cover skin when outdoors and remove these before going indoors, where possible.
They should tuck their pants into their socks and wear long sleeved tops if possible.
Consider having an ether containing spray in the first aid kit when engaging in activities in areas where ticks may be present.
Animal allergy
Some animal feed contains food allergens (such as nuts in birdseed and cow feed, milk and egg in dog food, fish in fish food, peanut butter in dog food, fish in cat food). If possible, source animal feed that does not contain foods that children are allergic to.
Children with egg allergy should only handle chicks that hatched the previous day or longer (no wet feathers) and must wash their hands afterwards. Further information is available from Allergy & Anaphylaxis Australia.
Exposure to animals such as domestic dogs, cats, rabbits, rats, mice, guinea pigs and horses may trigger contact dermatitis (rashes), eczema, allergic rhinitis (hay fever) and sometimes asthma.
Anaphylaxis to animals such as horses or dogs is rare but may occur and should be considered with activities such as “show and tell”, or visits to farms or zoos.
Food allergy
Do not use sunscreen containing any food products (such as nut oils, cow’s or goat’s milk).
Children may be allergic to foods grown in the garden (it is possible to be allergic to any food including fruits and vegetables). Talk to parents/guardians if new foods are being introduced.
Mulches used for gardens can contain food allergens (such as peanut shells) and mould allergens. If possible, source mulches that do not contain allergens and store in a dry place to minimise the growth of moulds.
Special events
Children should not miss out on activities because of their food allergy, however they (or the CEC service as a whole) may have to do things slightly differently to increase safety.
Special events such as picnics are high risk for children with food allergy as staff can be distracted. Speak with parents/guardians of children with food allergy to see if they (or a trusted relative) may be able to attend as a volunteer to supervise the child.
Consider children with food allergy when planning any fundraisers, cultural days or stalls, breakfast mornings, picnics and other celebrations involving food.
Liaise with the parents/guardians of children with food allergies well in advance so they can provide suitable food, adjust the activity to accommodate the children with food allergies and/or plan to help on the day.
Send a notice home to all parents/guardians prior to the event outlining that one or more children at the service have food allergies and request that these foods are avoided where possible.
Children with food allergy should not consume any food brought in by other children/families even if they are thought to be safe.
Children with food allergy can participate in birthday celebrations if their parents/guardians supply a safe ‘treat box’ or safe cupcakes that are stored in the service freezer in a labelled sealed container, to prevent cross contamination.
Medications, creams and latex
Any medication administered in the CEC service should be given in accordance with service guidelines, policy and procedures, and with the written permission of parents/guardians.
Some soaps, nappy creams and moisturisers contain allergens.
Encourage parents/guardians of children with food allergy to supply their own skin treatments or ask them to check the ingredients of CEC service supplies.
Staff do not have to restrict creams and/or makeup they put on at home.
Do not use sunscreen containing food products (such as nut oils, cow’s or goat’s milk).
Use non-latex gloves at nappy changing stations, in first aid kits and in kitchens.
Food for children with latex allergy should be prepared with clean hands or non-latex gloves.
Non-latex balloons should be used when there is a child with latex allergy.
First aid kits should have non-latex sticking plasters and non-latex gloves available.
This information has been adapted from a table that was initially produced by Allergy & Anaphylaxis Australia (A&AA). To ensure consistency of information A&AA, Australasian Society of Clinical Immunology and Allergy (ASCIA) and the National Allergy Council endorse these anaphylaxis risk minimisation strategies.
Disclaimer
This document has been developed by A&AA, ASCIA and the National Allergy Council and has been peer reviewed by ASCIA members. It is based on expert opinion and the available published literature at the time of review. Information contained in this document is not intended to replace medical advice and any questions regarding a medical diagnosis or treatment should be directed to a medical practitioner.
The development of this document is not funded by any commercial sources and is not influenced by commercial organisations.
Content updated July 2025.